Single-Blind Food Challenge Test for Food Sensitivity is one of the best practices in the diagnosis of food intolerance and it is inferior only to the double-blind placebo-controlled food challenge model.
Benefits
Single-Blind Food Challenge Test can help to determine if food sensitivities are contributing to behavioral and cognitive disorders.
It is a useful guide for structuring elimination diets for children with neurological and behavioral disorders (such as Autism Spectrum Disorder, hyperactivity, attention deficits, and other related conditions).
Without proper testing, children may continue to be fed with offending foods unaware of their adverse effects or, conversely, be deprived of foods which is actually safe for them to eat.
Elimination of offending foods may improve the child’s health and behavior. Whereas unnecessary food restrictions may lead to nutritional imbalances that can worsen symptoms of autism and hyperactivity.
Why this testing method is more accurate than other tests?
Scientific research has repeatedly shown that the food challenge methods are the only reliable testing for food sensitivities.
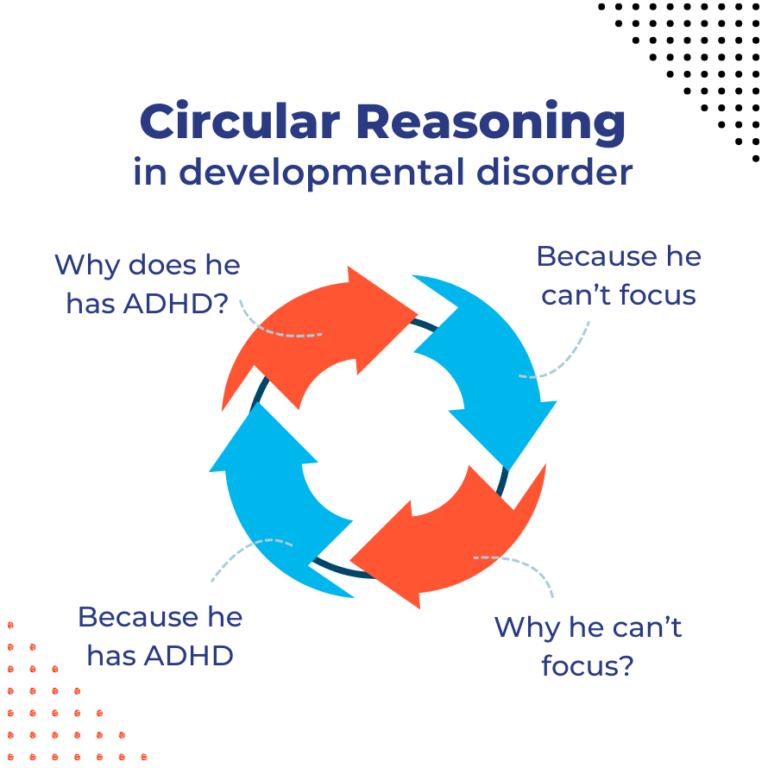
During the test, the person evaluating the behavioral effects of the diet does not know if the food has been given or not (technically, the assessor is blind). A blind assessor greatly reduces the risk of confirmation biases, cognitive errors that are common when no formal testing method is implemented.
Other testing methods, such the infamous IgG tests, are not only unable to identify harmful foods but generate a very high number of false positive (i.e. safe foods wrongly identified as an allergen). The use of these discredited tests can lead to unnecessary and harmful dietary restriction.
How does it work?
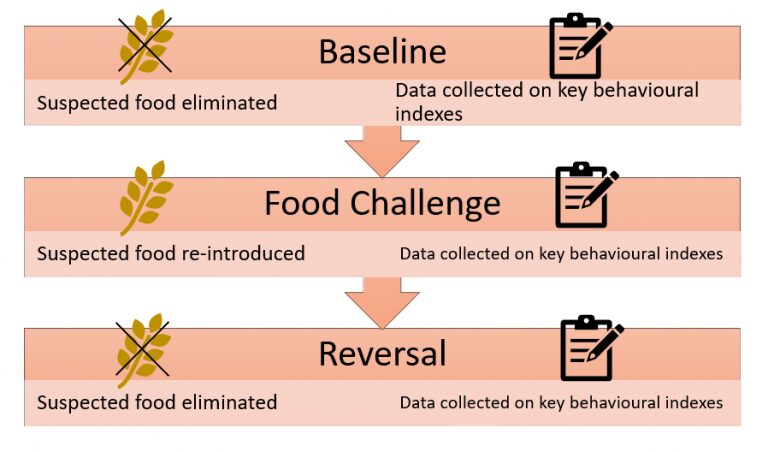
The test involves 3 phases: Baseline, Food Challenge, and Reversal. The suspected food is only administered to the child during the Food Challenge phase, whereas during Baseline and Reversal the food is eliminated from child’s diet.
During each phase data are collected on one or more key behavioral indexes. Depending on the child condition, the indexes to be measured may vary. For an hyperactive child may be ‘time spent off task’ or ‘time spent out of the chair’, for an child with Autism may be ‘frequency of eye contact’ or ‘engagement in social interaction’. Each of index is operationally defined in observable terms.
How are results interpreted?
The variation in the distribution of the behavioral indexes measured are plotted into chart and a visual analysis is conducted to evaluate the strength of the correlation between the indexes measured and the suspected food. Higher levels in the key behavioral indexes are suggestive of sensitivity to the food.